Our health journey often brings us to moments where general advice isn’t enough. We need focused, expert attention. This is where specialized medical care becomes essential. It provides custom solutions for complex health needs, helping us achieve and maintain personal well-being.
In this extensive guide, we will explore specialized medical care. We will cover its definition, how it differs from primary care, and the many examples of specialties available today. We will also look at the crucial role of care coordination, ensuring all our health providers work together.
We will also highlight key advancements changing how we receive care. This includes innovations in urological health and the rise of aesthetic and reconstructive medicine. We will also examine the growing importance of palliative care for serious illnesses. As we seek more comprehensive health solutions, understanding how specialized medical care can include Integrative Specialized Medical Care is vital.
Finally, we will offer practical advice on navigating your path to specialized care. We will discuss financial considerations and glimpse into the future of personalized medicine. Our goal is to empower you with knowledge.
Understanding the landscape of modern healthcare begins with distinguishing between primary care and specialized medical care. While both are integral to our health, their roles, focus, and expertise differ significantly.
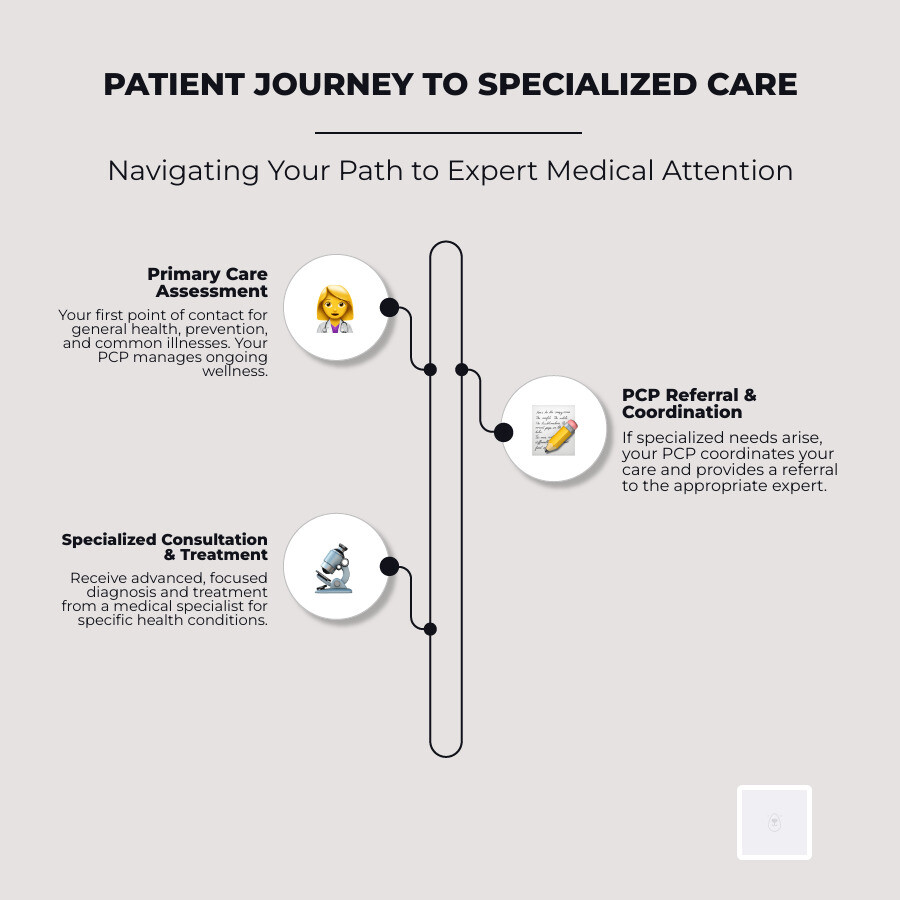
Primary care serves as our first point of contact with the healthcare system. It encompasses a broad range of services focused on prevention, wellness, and the treatment of common illnesses. Primary care providers (PCPs) — including doctors, nurses, nurse practitioners, and physician assistants — typically maintain long-term relationships with patients, offering continuous care and advice on a wide spectrum of health issues. They are our trusted guides, often coordinating our care and referring us to specialists when needed.
Specialized medical care, on the other hand, digs deeper into specific areas of medicine, addressing particular conditions, diseases, or patient populations. These services are provided by healthcare professionals who have undergone advanced training and possess expertise beyond general medical practice. Unlike PCPs who manage general health, specialists concentrate on diagnosing, treating, and managing complex or rare conditions within their niche. This advanced focus is reflected in compensation, with specialists earning significantly more than primary care physicians. According to the 2022 Medscape Physician Compensation Report, primary care physicians earned an average of $260,000 annually, while specialists commanded an average of $368,000.
The distinction between these two forms of care is crucial for effective healthcare navigation. While our PCP acts as the general contractor for our health, a specialist is the skilled artisan brought in for specific, intricate tasks.
Here’s a table comparing Primary Care vs. Specialized Care on key aspects:
Aspect Primary Care Specialized Medical Care Scope Broad, general health, prevention, common illnesses Narrow, specific conditions, diseases, or body systems Training General medical education, family medicine, internal medicine, pediatrics Advanced, in-depth training (residency, fellowship) in a specific field Patient Relationship Long-term, continuous, holistic Episodic, focused on a specific issue, often referral-based Typical Conditions Colds, flu, routine check-ups, chronic disease management (e.g., mild diabetes, hypertension) Cancer, complex heart disease, neurological disorders, specific surgical needs Providers General practitioners, family doctors, internists, pediatricians, nurse practitioners Cardiologists, oncologists, neurologists, surgeons, endocrinologists, dermatologists Key Components and Examples of Specialties
The medical field is vast, and specialized medical care reflects this diversity, with numerous branches dedicated to specific areas of human health. These specialties can be classified in various ways: by the organ system they focus on, the age range of patients they treat, whether they are diagnostic or therapeutic, or if they involve surgical or internal medicine approaches.
Some of the most common medical specialties we encounter include:
- Cardiology: Focuses on heart and blood vessel disorders.
- Oncology: Deals with the diagnosis and treatment of cancer.
- Neurology: Specializes in disorders of the nervous system, including the brain, spinal cord, and nerves.
- Orthopedics: Addresses conditions affecting bones, joints, ligaments, tendons, and muscles.
- Urology: Concentrates on the urinary tract and male reproductive organs.
- Dermatology: Specializes in skin, hair, and nail conditions.
- Gastroenterology: Deals with the digestive system and its disorders.
- Endocrinology: Focuses on hormone-related conditions like diabetes and thyroid disorders.
- Pediatrics: Provides medical care for infants, children, and adolescents.
- Geriatrics: Specializes in the healthcare of elderly people.
- Rheumatology: Treats rheumatic diseases, which affect joints, muscles, and bones.
- Ophthalmology: Deals with eye diseases and vision care.
- Otolaryngology (ENT): Focuses on conditions of the ear, nose, and throat.
- Psychiatry: Specializes in mental health disorders.
These examples illustrate how specialties can be organ-based (like cardiology for the heart), technique-based (like radiology for imaging), or patient-population-based (like pediatrics for children). The continuous evolution of medical knowledge and technology means new sub-specialties are constantly emerging, further refining the precision and effectiveness of care.
The Crucial Role of Care Coordination
In an increasingly specialized healthcare system, care coordination emerges as a cornerstone of effective patient management. Care coordination refers to the deliberate organization of patient care activities between two or more participants (including the patient) involved in a patient’s care to facilitate the appropriate delivery of healthcare services. It’s about ensuring that all our healthcare providers are on the same page, working towards a common goal for our well-being.
The importance of communication between providers cannot be overstated, especially for patients with multiple health issues. Without proper coordination, different specialists might prescribe conflicting medications, order redundant tests, or develop treatment plans that don’t account for a patient’s overall health picture, social needs, or lifestyle. This fragmentation can lead to confusion, increased costs, and potentially adverse health outcomes.
Our primary care provider often plays a pivotal role as the care coordinator, acting as the central hub for all our health information. They can synthesize information from various specialists, ensuring that treatments are complementary and aligned with our overall health goals. For instance, consider Maria, a 68-year-old with diabetes who experienced worsening vision. Her primary care provider, in coordination with her endocrinologist, adjusted her medication, connected her with food services and a nutritionist, and referred her to an ophthalmologist, while also arranging transportation. This holistic approach, facilitated by strong care coordination, addressed her medical needs and her health-related social needs.
The benefits of robust care coordination for patient outcomes are profound. It leads to better health outcomes by ensuring comprehensive and integrated care, reduces medical errors by minimizing conflicting treatments, and provides a holistic patient view that considers all aspects of an individual’s health and life circumstances. This integrated approach is a fundamental aspect of Integrative Specialized Medical Care, where various treatments and perspectives are brought together for optimal patient benefit. It ensures that our journey through specialized care is smooth, efficient, and ultimately, more effective in achieving our personal well-being.
Key Areas of Advancement in Specialized Medical Care
The field of specialized medical care is in a constant state of evolution, driven by relentless technological innovation, the development of new treatment modalities, and a fundamental shift towards more patient-centered models. These advancements are not just incremental improvements; they are changing how we diagnose, treat, and manage complex health conditions, significantly enhancing our personal well-being.
One of the most impactful advancements is the integration of cutting-edge technology. From advanced imaging techniques that offer unprecedented views inside the human body to sophisticated surgical robots that enable minimally invasive procedures, technology is making specialized care more precise and less burdensome. Remote monitoring, for example, has emerged as a game-changer, allowing healthcare providers to track vital signs, cardiac activity, and other critical health data from a distance. This capability is not merely convenient; it’s life-saving. Statistics show that remote monitoring can lead to a remarkable 50% mortality reduction, particularly in conditions like heart disease, which accounts for 25% of all deaths in the U.S.A., with 47% of sudden cardiac deaths occurring outside a hospital. This highlights the critical role of accessible and continuous monitoring in preventing adverse events.

Improved diagnostic accuracy is another significant area of advancement. Innovations in genetic testing, biomarker identification, and artificial intelligence (AI)-powered diagnostic tools are enabling earlier and more precise diagnoses. This means treatments can be initiated sooner and be more targeted, leading to better prognoses and a higher quality of life. The shift towards patient-centered models emphasizes individual needs, preferences, and values, ensuring that specialized care is not just medically effective but also aligned with our personal goals and comfort.
Innovations in Urological Health
Urological health is a prime example of a specialized field that has seen remarkable innovations, significantly improving the quality of life for countless individuals. Conditions ranging from prostate issues and kidney stones to erectile dysfunction and urinary incontinence, once managed with limited options, now benefit from a suite of advanced treatments.
Minimally invasive procedures have revolutionized urology. Techniques like laparoscopic and robotic-assisted surgery allow for complex operations to be performed through small incisions, leading to reduced pain, shorter hospital stays, and faster recovery times. This is particularly beneficial for conditions such as prostate cancer, where robotic prostatectomy has become a gold standard, offering improved precision and better functional outcomes.
Advancements in treating common conditions have also been transformative. For erectile dysfunction (ED), new oral medications, injectable therapies, and external devices continue to evolve, while innovative approaches like shockwave therapy and specialized injections are showing promising results in restoring natural function. Similarly, urinary incontinence, a condition that significantly impacts daily life, now has a broader range of effective treatments, including advanced medications, pelvic floor therapies, and minimally invasive surgical solutions like slings and artificial sphincters.
The focus in modern urology is not just on treating the disease but profoundly on enhancing the patient’s quality of life. For those seeking comprehensive and modern approaches to male sexual health, including advanced therapies for ED and other urological concerns, exploring a resource about modern specialized urologic care can provide valuable insights into the latest treatments and personalized care options available. These innovations underscore the commitment of specialized medical care to not only prolong life but also to ensure that life is lived with dignity and comfort.
The Rise of Aesthetic and Reconstructive Specialties
Beyond the traditional scope of internal medicine and surgery, specialized medical care also encompasses fields dedicated to enhancing appearance and restoring function, known as aesthetic and reconstructive specialties. While often associated with cosmetic improvements, these fields play a crucial role in personal well-being by addressing both physical and psychological needs.
Reconstructive surgery, for instance, is far more than just “cosmetic.” It is a vital branch of medicine focused on restoring form and function to parts of the body affected by birth defects, trauma, disease (such as cancer removal), or burns. This can involve intricate procedures like breast reconstruction after mastectomy, facial reconstruction after an accident, or limb reconstruction, all of which profoundly impact a patient’s physical capabilities and self-esteem. The goal is to help individuals regain a sense of normalcy and improve their quality of life after life-altering events.
The aesthetic side, while sometimes elective, also contributes significantly to well-being. Procedures aimed at improving appearance can boost confidence, reduce self-consciousness, and align an individual’s external appearance with their internal self-perception. This often involves non-invasive techniques, which have seen a surge in popularity and effectiveness.

The integration of technology has been a game-changer in these specialties. Advanced imaging allows for precise planning, while laser technologies, injectables, and energy-based devices offer sophisticated, minimally invasive options for skin rejuvenation, body contouring, and hair restoration. The growing field of advancements in specialized cosmetic medical care is a testament to how these specialties are continuously innovating to provide safer, more effective, and more personalized solutions. These advancements highlight a holistic understanding of health, recognizing that physical appearance and self-perception are integral components of overall personal well-being.
A Holistic Approach to Managing Serious Illness
When facing a serious illness, the focus often shifts from cure to comfort, from battling disease to preserving dignity and quality of life. This is precisely where palliative care steps in, offering a holistic approach to managing serious illness that complements curative treatments.
Palliative care is specialized medical care for people living with a serious illness, regardless of their prognosis. Its primary goal is to provide relief from the symptoms and stress of the illness, aiming to improve quality of life for both the patient and their family. It is distinct from hospice care, which is typically reserved for individuals with a life expectancy of six months or less who are no longer seeking curative treatments. Palliative care, conversely, can be provided at any age and at any stage of a serious illness, often alongside curative treatments.
The benefits of palliative care are well-documented. Numerous studies consistently show that palliative care significantly improves patient quality of life and lowers symptom burden. Palliative care specialists excel at managing complex physical and emotional symptoms, including pain, depression, anxiety, fatigue, shortness of breath, constipation, nausea, loss of appetite, and difficulty sleeping. They also provide skilled communication about future expectations, helping patients and families align care with their goals and priorities.

A specially-trained team of doctors, nurses, social workers, and chaplains provides this extra layer of support, working in partnership with the patient’s primary physicians. This team approach ensures that all aspects of a patient’s well-being—physical, emotional, social, and spiritual—are addressed.
The growth of palliative care has been significant. Today, more than 1,700 hospitals with 50 or more beds have a palliative care team, and its reach is expanding beyond the hospital into community settings. This expansion is crucial as it allows more patients to benefit from this compassionate care in familiar environments. Conditions commonly associated with the need for palliative care include:
- Cancer
- Heart disease
- Chronic lung disease (e.g., COPD, cystic fibrosis)
- Kidney or liver failure
- Advanced dementia
- Multiple Sclerosis (MS)
- Amyotrophic Lateral Sclerosis (ALS)
By integrating palliative care with curative treatments, we ensure that patients receive comprehensive support that not only addresses their disease but also prioritizes their comfort, dignity, and overall well-being throughout their illness journey.
Navigating Your Path to Specialized Care
Starting on a journey through specialized medical care can feel daunting, but understanding how to steer this path effectively empowers us to make informed decisions for our health.
The first step often involves getting a referral. While some insurance plans (like PPOs) may allow direct access to specialists, many (especially HMOs) require a referral from your primary care physician (PCP). Your PCP is crucial here; they can assess your symptoms, conduct initial tests, and determine if a specialist is indeed necessary. They can also recommend specialists within your insurance network who are best suited for your specific condition. Always check your insurance policy regarding referral requirements to avoid unexpected costs.
Choosing the right specialist is paramount. Beyond a referral, consider factors like the specialist’s experience with your specific condition, their communication style, and their location. Board certification is a key indicator of a physician’s qualifications and expertise in a specialty. The American Board of Medical Specialties (ABMS) certifies physicians who have demonstrated mastery of core knowledge and skills in their field, and looking for this credential can provide assurance of quality care. Online reviews and recommendations from trusted sources can also be helpful, but always prioritize professional credentials and your comfort level.
Preparing for your appointment can significantly improve its effectiveness. Gather all relevant medical records, including test results, medication lists, and a detailed history of your symptoms. Write down a list of questions you want to ask your specialist. This ensures you cover all your concerns and don’t forget important details during the consultation.
Questions to ask your specialist might include:
- What is my diagnosis?
- What are the treatment options, and what are their pros and cons?
- What are the potential side effects or risks of treatment?
- How will this treatment impact my daily life?
- What is the expected outcome of treatment?
- Are there any alternative treatments or clinical trials I should consider?
- How will you coordinate my care with my other doctors?
The patient’s role as an advocate for their own health is critical. Don’t hesitate to ask for clarification, express your concerns, or seek a second opinion if you feel it’s necessary. Understanding your treatment options thoroughly and actively participating in decision-making ensures that your care aligns with your values and goals. Specialized medical care is a partnership between you and your healthcare team.
Understanding the Financials of Specialized Medical Care
The financial aspect of specialized medical care is a significant concern for many patients. Navigating insurance coverage, understanding costs, and recognizing the broader economic impact of specialized care are all crucial components of personal well-being.
Insurance coverage is the primary determinant of out-of-pocket expenses. It’s essential to understand your plan’s specifics, particularly regarding in-network versus out-of-network specialists. Seeing an out-of-network provider can lead to substantially higher costs, as your insurance may cover a smaller percentage or none at all. Deductibles, co-pays, and co-insurance also play a role, so familiarizing yourself with these terms before seeking specialized care is advisable. Many plans require pre-authorization for certain specialized procedures or treatments, and failing to obtain this can result in denied claims.
The financial landscape also highlights the physician salary differences between generalists and specialists. As noted earlier, specialists generally earn more than primary care physicians due to their extensive training and the complex nature of their work. While primary care physicians earn an average of $260,000 annually, specialists earn an average of $368,000. These figures reflect the investment in specialized education and the demand for highly focused expertise.
From a broader perspective, system-level cost benefits of coordinated care are increasingly recognized. Fragmented care, where specialists operate in silos, can lead to redundant tests, unnecessary procedures, and prolonged treatment durations, all of which drive up healthcare costs. Effective care coordination, as championed by initiatives like those from the CMS Innovation Center, aims to streamline patient pathways, reduce inefficiencies, and ultimately lower overall healthcare expenditures while improving outcomes. This is not just theoretical; studies consistently show improvements in both quality measures and resource utilization once coordinated care, including palliative care, is introduced, potentially lowering costs for both patients and the healthcare system.
Specifically, palliative care cost reduction is a unique insight. While focused on quality of life, palliative care can also lead to significant cost savings. By providing expert symptom management and aligning care with patient goals, it can reduce unnecessary hospitalizations, emergency room visits, and aggressive treatments that may not improve outcomes in serious illness. This demonstrates that patient-centered, quality-focused care can also be economically advantageous.
Understanding these financial implications allows us to better plan for and manage the costs associated with specialized medical care, ensuring that financial burdens do not impede access to necessary and beneficial treatments.
The Future of Personalized Specialized Medical Care
The horizon of specialized medical care is brimming with transformative possibilities, promising an era of even more personalized, precise, and accessible healthcare. Several key trends are converging to shape this future, moving us closer to a healthcare system truly custom to the individual.
Genomic medicine stands at the forefront of this revolution. By analyzing an individual’s unique genetic code, specialists can identify predispositions to certain diseases, predict responses to medications, and develop highly targeted therapies. This allows for preventive strategies and treatments that are precisely matched to a patient’s biological makeup, moving beyond a one-size-fits-all approach.
Artificial intelligence (AI) in diagnostics is rapidly advancing, offering unprecedented capabilities for early and accurate disease detection. AI algorithms can analyze vast amounts of medical data, including imaging scans, pathology reports, and patient histories, to identify subtle patterns that human eyes might miss. This augments the diagnostic abilities of specialists, leading to quicker diagnoses and more effective treatment plans.
The expansion of telehealth has already demonstrated its immense potential, particularly in specialized care. Remote consultations, virtual follow-ups, and digital monitoring platforms break down geographical barriers, making specialized expertise accessible to patients in remote areas or those with mobility challenges. This trend is expected to continue, enhancing convenience and continuity of care.
The healthcare system is also shifting towards value-based care models. These models incentivize healthcare providers to focus on patient outcomes and overall health rather than simply the volume of services provided. This aligns perfectly with specialized care, encouraging coordinated, efficient, and effective treatments that deliver real value to patients. The CMS Innovation Center, for example, is actively exploring strategies to support person-centered, value-based specialty care.
Furthermore, we are witnessing a significant growth of community-based specialty care. Palliative care, for instance, is increasingly spreading beyond hospitals into community settings, making it more accessible to patients in their homes or local clinics. This decentralization of specialized services aims to integrate care more seamlessly into patients’ daily lives, reducing the burden of travel and improving convenience.
Finally, there’s an increased focus on prevention and wellness within specialties. While specialists traditionally treat existing conditions, there’s a growing recognition that specialized knowledge can also be applied to proactive prevention. For example, cardiologists might work more closely with patients at high risk of heart disease to implement lifestyle interventions, or oncologists might advise on genetic screening and early detection strategies. This holistic view ensures that specialized medical care is not just reactive but also plays a vital role in maintaining long-term health and well-being.
Frequently Asked Questions about Specialized Medical Care
What is the main difference between a primary care physician and a specialist?
A primary care physician provides general, long-term care for a wide range of health issues and is often your first point of contact. They focus on prevention, wellness, and common illnesses. A specialist, on the other hand, has advanced training and expertise in a specific area of medicine, such as cardiology or oncology, and focuses on diagnosing and treating conditions related to that particular field.
Can I see a specialist without a referral?
This depends on your health insurance plan. Many Health Maintenance Organization (HMO) plans require a referral from your primary care provider to see a specialist, while Preferred Provider Organization (PPO) plans may allow you to self-refer, though sometimes at a higher cost. It’s always best to check your specific insurance policy or contact your insurance provider to understand their requirements and coverage for specialist visits.
How does palliative care work with my regular treatments?
Palliative care is designed to work alongside and complement your curative treatments, not replace them. It provides an extra layer of support focused on relieving symptoms, stress, and pain associated with your serious illness, helping you better tolerate and benefit from your primary treatments. The palliative care team collaborates closely with your other doctors to ensure your overall well-being is addressed while you continue to pursue curative therapies. It’s appropriate at any age and at any stage of a serious illness.
Conclusion
As we’ve explored, specialized medical care is a dynamic and indispensable component of our modern healthcare system, continually evolving to meet complex health needs and improve personal well-being. We’ve seen how it differentiates from primary care, offering deep expertise in specific medical domains, and how crucial care coordination is in stitching together a cohesive and effective treatment plan.
The advancements in specialized medicine are truly remarkable, from innovations in urological health and the rise of aesthetic and reconstructive specialties to the compassionate and holistic approach of palliative care. These developments, fueled by technology and a commitment to patient-centered models, are changing how we experience healthcare.
Navigating this intricate landscape requires us to be informed and proactive, understanding the roles of different providers, the financial implications, and the ever-expanding possibilities of personalized medicine. By empowering ourselves with knowledge, we can actively participate in our healthcare decisions, ensuring that our path to well-being is supported by the most appropriate and advanced specialized care available. The future of personal well-being, we believe, lies in this integrated, innovative, and deeply personalized approach to medicine.





